The Cost Of Creating A New Drug Now $5 Billion, Pushing Big Pharma To Change
There’s one factor that, as much as anything else, determines how many medicines are invented, what diseases they treat, and, to an extent, what price patients must pay for them: the cost of inventing and developing a new drug, a cost driven by the uncomfortable fact than 95% of the experimental medicines that are studied in humans fail to be both effective and safe.
A new analysis conducted at Forbes puts grim numbers on these costs. A company hoping to get a single drug to market can expect to have spent $350 million before the medicine is available for sale. In part because so many drugs fail, large pharmaceutical companies that are working on dozens of drug projects at once spend $5 billion per new medicine.
“This is crazy. For sure it’s not sustainable,” says Susan Desmond-Hellmann, the chancellor at UCSF and former head of development at industry legend Genentech, where she led the testing of cancer drugs like Herceptin and Avastin. “Increasingly, while no one knows quite what to do instead, any businessperson would look at this and say, ‘You can’t make a business off this. This is not a good investment.’ I say that knowing that this has been the engine of wonderful things.”
A 2012 article in Nature Reviews Drug Discovery says the number of drugs invented per billion dollars of R&D invested has been cut in half every nine years for half a century. Reversing this merciless trend has caught the attention of the U.S. government. Francis Collins, the director of the National Institutes of Health, in 2011 started a new National Center for Advancing Translational Sciences to remove the roadblocks that keep new drugs from reaching patients.
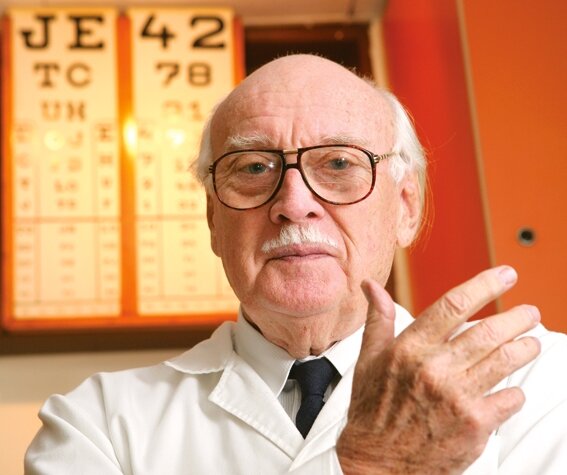
“One point your numbers tell you is how horrendous the failure rate is and how that causes the cost of success to be so much higher,” says Collins. “We would love to contribute to making that failure rate lower, to identifying those bottlenecks and to trying to reengineer the pipeline so if failures happen, they happen very early and not in later stages where the costs are higher.”
The good news is that a close look at the data we collected provides some hints as to how to improve the industry’s hit rate – and how individual companies, without lowering the overall cost of developing a drug, can at least reduce their own expenses. Some companies – like Bristol-Myers Squibb, Regeneron Pharmaceuticals, and Aegerion – do far better than their peers.
Fighting The Law Of Averages
Where do my estimates come from? Using data from the Innothink Center for Research in Biomedical Innovation, I tabulated the number of brand new drugs launched by 98 publicly traded biotechnology and drug companies over the past decade. Then, using FactSet Systems, I tallied each company’s research and development spending over the ten years preceding their most recent drug approval. Then I divided the second number by the first. (Again, the whole list and methodology is here.)
Sixty-six of the 98 companies studied launched only one drug this decade. The costs borne by these companies can be taken as a rough estimate of what it takes to develop a single drug. The median cost per drug for these singletons was $350 million. But for companies that approve more drugs, the cost per drug goes up – way up – until it hits $5.5 billion for companies that have brought to market between eight and 13 medicines over a decade.
| Number of drugs approved |
R&D cost per drug ($MIL) |
| Median |
Mean |
| 8 to 13 |
5459 |
5998 |
| 4 to 6 |
5151 |
5052 |
| 2 to 3 |
1803 |
2303 |
| 1 |
351 |
953 |
| Sources: Innothink Center For Research In Biomedical Innovation; FactSet Systems. |
Why? For every small company that succeeds, there are many more that fail. A big pharmaceutical company carries that weight of failure, with both its successes and its failures on the books.
Why Does Big Pharma Spend So Much?
Some caveats, though: drug companies have tax incentives to count costs in research and development, which could inflate the figure; they also are likely to spend extra money in order to get those medicines approved in other countries. Even more important is the fact that some R&D costs come from monitoring the safety of medicines after they become hits to monitor reports of side effects. “Our safety infrastructure is close to 1,000 people,” says Paul Stoffels, the co-chairman of pharmaceuticals at Johnson & Johnson, which had the most new drugs approved and spent $5.2 billion per drug. “That is a whole biotech company and it is also part of our R&D budgets.”
Also, a small company cannot spend enough to pay for a $1 billion-plus program for a heart drug, as Pfizer, Roche, and J&J have, or for an Alzheimer’s medicine. But if such a drug succeeds, the payoff can be enormous – see Pfizer’s Lipitor, which is now generic but which had annual sales of $11 billion. Bigger drugs can be more expensive to develop.
| 10 Year R&D Spending ($MIL) |
R&D Spending Per Drug ($MIL) |
| Median |
Mean |
| >20,000 |
6348 |
6632 |
| >5,000 |
2883 |
2961 |
| >2,000 |
1917 |
2480 |
| >1,000 |
1459 |
741 |
| Sources: Innothink Center For Research In Biomedical Innovation; FactSet Systems |
Size has a cost. The data support the idea that large companies may be spend more per drug than small ones. Companies that spent more than $20 billion in R&D over the decade spent $6.3 billion per new drug, compared to $2.8 billion for those that had budgets of between $5 billion and $10 billion. Some CEOs, notably Christopher Viehbacher at Sanofi, have faced low R&D productivity in part by cutting the budget. This may make sense in light of this data. But it is worth noting that the bigger firms brought twice as many drugs to market. It still could be that the difference between these two groups is due to smaller companies not bearing the full financial weight of the risk of failure.
Clear Winners
Among big pharmaceutical companies, there is a clear standout: Bristol-Myers, which under former research chief Elliott Sigal focused on understanding human genetics and using the immune system as a weapon against cancer. The result has been 9 drug approvals, including Yervoy for melanoma and Orencia for rheumatoid arthritis, at a per drug cost of just $3.4 billion, half that of Eli Lilly or Pfizer. “Look at what he accomplished,” says Desmond-Hellmann. “Holy cow.”
J&J, Novo-Nordisk, and Amgen also perform well, as do smaller companies like Regeneron, Gilead, and Biogen Idec.
One common mistake is allowing projects to linger on when the odds of success have become low, says Roger Perlmutter, who ran Amgen’s R&D and is now doing the same thing at Merck. Another problem, he argues, is CEOs believing they can order up another drug like their last big hit, instead of following the science.
“Great drugs build great franchises, but great franchises don’t necessarily build great drugs,” Perlmutter says. “If you are too prescriptive with your R&D, you can spend an awful lot of money and not be terribly productive because there may actually not be any new mechanisms that you can get to right now that will help you in a particular disease area.”
Another successful strategy is to focus on ultra-rare diseases; treatments for such ailments can cost $200,000 or more per patient per year, and be highly lucrative. But these drugs don’t seem to eat up much in the way of R&D money. Genzyme, bought by Sanofi for $20 billion in 2011, spent $963 million per new drug. Alexion, the biggest stand-alone orphan drug maker,spent $490 million in R&D in the decade before its drug was approved; BioMarin, another orphan drug maker, spent just $134 million per drug.
The Power Of ‘Who Pays?’
 But reducing how much it costs to develop a new drug isn’t the only way to reduce a company’s cost. Another method: get somebody else to pay.
But reducing how much it costs to develop a new drug isn’t the only way to reduce a company’s cost. Another method: get somebody else to pay.
Many biotechnology companies benefit from deals in which a big pharma partner does some of the heavy lifting, for instance designing and running big clinical trials to prove a drug’s worth. But small companies have also benefited by adopting drugs that were abandoned by the companies that invented them. Cubist Pharmaceuticals spent $220 million in R&D before its antibiotic, hit the market. But the drug, Cubicin, was invented at Eli Lilly, which put significant resources into developing it before abandoning it. Aegerion last year launched a new heart drug for patients with a rare genetic disease that causes super-high cholesterol; it had originally been developed by Bristol for heart patients, but abandoned because of side effects. Aegerion’s R&D cost to get over the goal line? Just $74 million. The total cost spent on the medicine may have been triple that.
Philanthropies like the Michael J. Fox Foundation and the Multiple Myeloma Research Foundation now commonly use the strategy of bearing early research costs to get pharma interested. In the most visible example, the Cystic Fibrosis Foundation paid for the early development of a medication against that disease, a lethal lung ailment, at Vertex Pharmaceuticals. The result: a rare disease drug, Kalydeco, that is effective in patients whose CF is caused by a specific genetic mutation. Kalydeco costs $294,000 per patient per year.
The NIH is consciously imitating this approach. Collins, the NIH director, put former Merck scientist Christopher Austin in charge of his translational medicine institute and empowered him to fund further academic development of drugs that Big Pharma had abandoned, this time trying to find new uses for them. The idea is to improve the hit rate. Robert Beall, the CF Foundation’s chief executive, warned them to think hard about whether they would try to limit the price of any drugs that result. Collins says that’s impossible. “It’s a non-starter,” says Collins. “Attaching government influence on the ultimate pricing is a way to kill the whole field.”
A Political Minefield
There is a long history of political controversy around drug industry claims about the expense of developing new medicines. Pharmaceutical companies have defended the prices of their drugs by pointing to past estimates of the cost of developing a new medicine. Most of these estimates, which took a bottom-up approach of estimating each step in the drug development process, came in far below the numbers I’m using here.
But this argument always had a sense of ridiculousness to it; it only works up to a point. A diamond might get more valuable if the path of transporting it to its eventual buyer were fraught with danger, but a lump of coal would not. At some point, drugs have to justify their own value. The cost of inventing medicines has become not a defense but an albatross; if costs don’t come down, drug companies are in trouble.
Luckily, there are signs of hope. The Food and Drug Administration seems to be approving more drugs, even working with companies to help remove red tape and speed drugs for particularly serious diseases to market. And new technologies offer hope. Stem cells may allow for better safety testing of drugs, DNA sequencing for faster ways of figuring out what drugs to try to make. Collins, at the NIH, talks about developing organs in the lab that could be used for testing experimental medicines. Many companies are very consciously trying to remake and rejuvenate their R&D laboratories.
Then again, a lot of technologies have come and gone in the drug industry, often with the promise of lowering the cost of inventing a medicine. Yet the cost has gone up regardless.
“There are so many ways to fail that you always feel that you’re ascending the steep part of the learning curve,” says Perlmutter. “You keep finding more and more ways of making mistakes that ultimately result in having to spend a lot of money and not getting products out.”
The article is the excellent work of Matthew Harper.
http://www.forbes.com/sites/matthewherper/2013/08/11/how-the-staggering-cost-of-inventing-new-drugs-is-shaping-the-future-of-medicine/
Pin It














 But reducing how much it costs to develop a new drug isn’t the only way to reduce a company’s cost. Another method: get somebody else to pay.
But reducing how much it costs to develop a new drug isn’t the only way to reduce a company’s cost. Another method: get somebody else to pay.